Are Menopause and Hypoestrogenic Symptoms the Same Thing?
Not exactly—let’s unpack the difference.
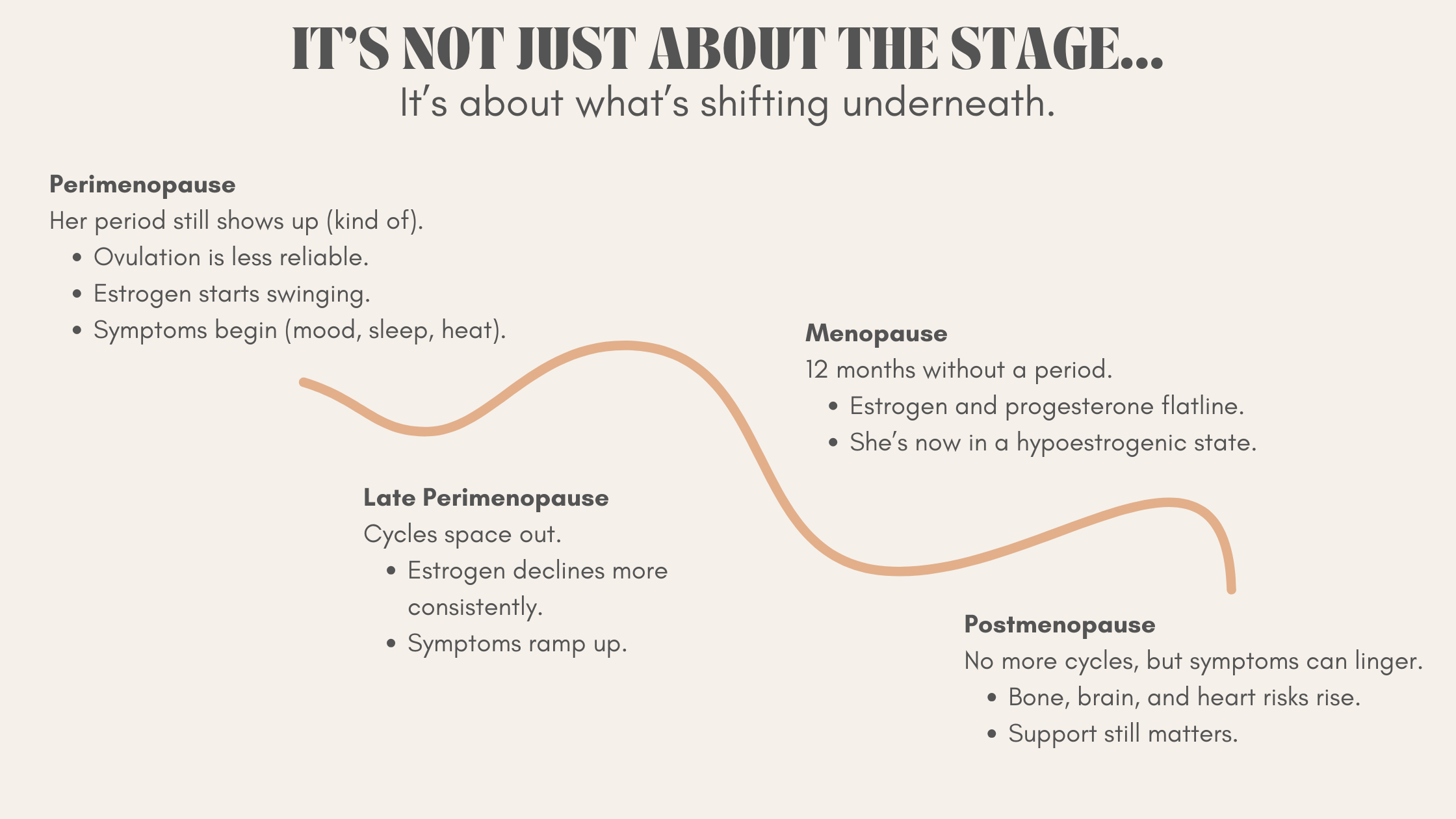
Menopause 101: Let’s Define the Stages First
here’s a lot of confusion about what menopause actually is, so let’s start there.
Menopause is the date of your last menstrual period. It’s a one-day event, technically speaking.
Perimenopause is the transitional time leading up to menopause. This can last years and is often when most of the chaos happens.
Postmenopause refers to everything after that final period.
Now, what’s actually going on during this transition?
To put it simply: ovarian function starts to shift, and eventually slows down.
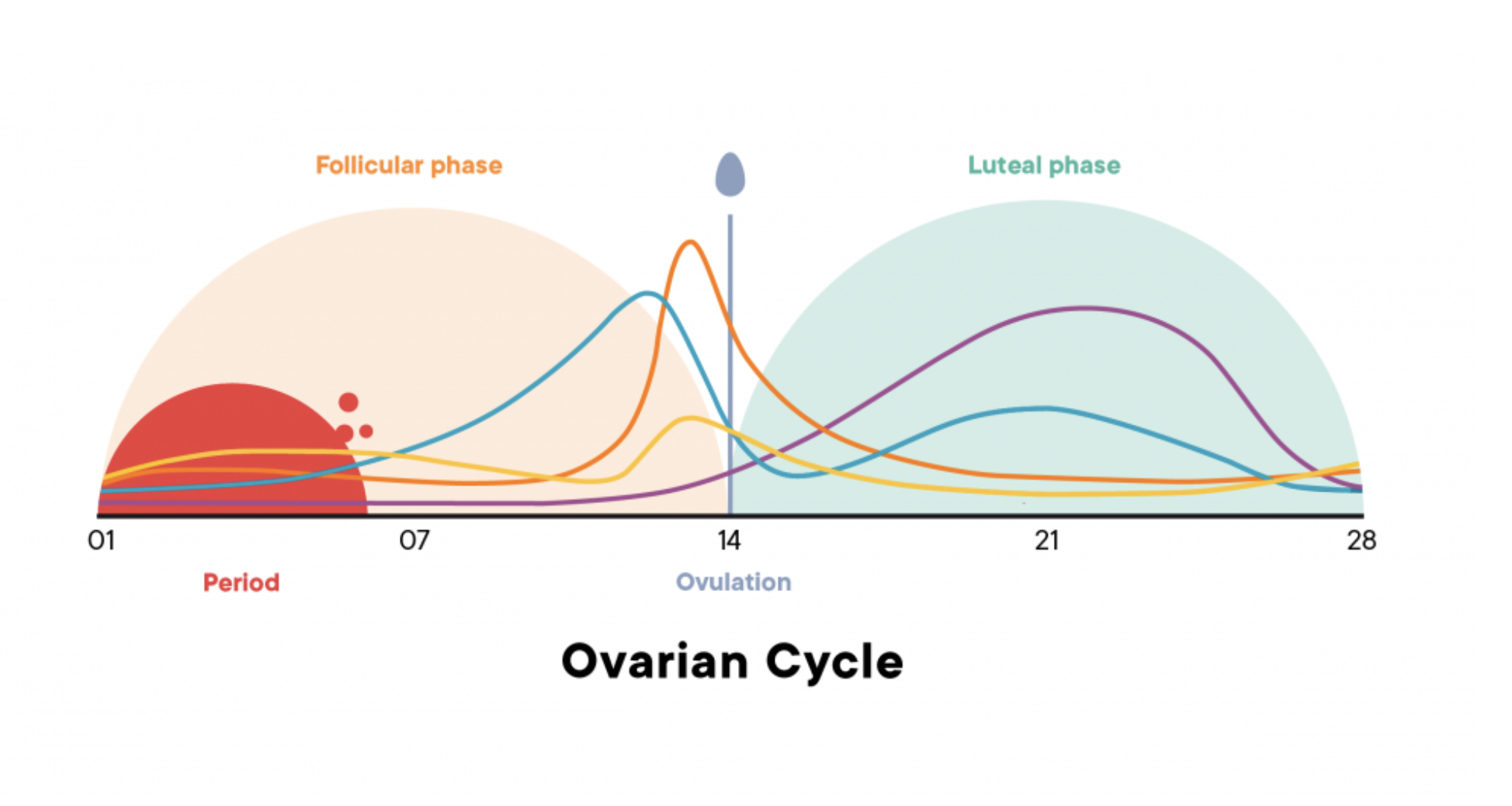
At first, this means ovulation becomes more irregular. You may skip ovulation some months. Progesterone levels start to weaken. Estrogen production still continues, but can become more erratic.
As the transition continues, estrogen starts to decline more significantly, until the ovaries eventually stop producing both estrogen and progesterone altogether.
This is what leads us into a hypoestrogenic state—a time when estrogen levels are low, flat, or inconsistent.
But here’s the important distinction:
You don’t need to be in menopause to have hypoestrogenic symptoms.
So What Are Hypoestrogenic Symptoms?
Hypoestrogenic symptoms are what most people associate with “menopause symptoms,” but they’re really about low estrogen, not just the menopause label itself.
The most common symptoms include:
Hot flashes
Night sweats
Vaginal dryness or discomfort
Sleep disturbances
Brain fog
Mood shifts
Low libido
Joint pain
Dry skin
And yes, these symptoms are common in menopause.
But they can also show up during:
Perimenopause, especially in the later stages
Postpartum and breastfeeding, due to estrogen suppression from high prolactin
Certain phases of the menstrual cycle, particularly just before a period when estrogen dips
Post-hysterectomy or surgical menopause
Medications or treatments that suppress estrogen production
Why This Distinction Matters
One of the most common frustrations I hear from patients is this:
“I’m still getting a period, so my doctor said it can’t be my hormones.”
Or worse: “My labs are normal, so I must be fine.”
Here’s what I want you to know.
Just because you're still bleeding doesn’t mean your estrogen levels are stable.
You can absolutely experience hypoestrogenic symptoms cyclically during perimenopause as your estrogen fluctuates.
In fact, many women report symptoms that feel predictable each month. For example:
You feel clear and calm mid-cycle
Then like a different person before your period: hot at night, irritable, anxious, and foggy
That drop in estrogen? It’s real—and it’s triggering symptoms.
What Treatment Might Look Like
Hypoestrogenic symptoms can be supported with hormone therapy—but that’s not always the first (or best) option for everyone.
For example:
In early perimenopause, you may not need full hormone therapy. You might benefit from targeted support for ovulation, like stress management, sleep support, or cyclic progesterone.
Postpartum or breastfeeding-related low estrogen may resolve as prolactin decreases over time.
In postmenopause, vaginal estrogen or systemic hormone therapy may be appropriate, depending on symptoms and personal risk.
The key is individualization.
We’re not just treating a stage—we’re treating you.
“Just because you’re still bleeding doesn’t mean your estrogen isn’t crashing.”
Final Thoughts: Treat the Symptoms, Not Just the Stage
Too many women are dismissed because their cycle hasn’t “officially stopped.”
But if you’re dealing with night sweats, mood swings, poor sleep, or brain fog, you don’t need to wait for a calendar date—or lab values—to get help.
Whether your symptoms are due to perimenopause, postpartum, or full-on menopause, the real question is:
What support will help you feel better now—and protect your long-term health?
Wondering if your symptoms are hormonal—even if you still get a period? Let’s talk. Book your consult today.