Why Menopause Care Needs More Than Hormones
Because relief is just the beginning.
Let’s Start With the Obvious: Hormones Are Having a Moment.
Scroll Instagram for five minutes and you’d think hormone therapy is the only thing that matters in perimenopause and menopause care.
And listen, I get it.
Hormone therapy can be transformational. For many women, it brings relief from brutal hot flashes, sleepless nights, mood swings, and the sense that they’ve lost themselves somewhere along the way.
But here’s what I want you to hear:
Hormone therapy is just the beginning—not the full story.
And if we stop the conversation there, we’re doing women a disservice.
The Incomplete Narrative
It’s like the online conversation starts the sentence but forgets to finish it.
Kind of like how your brain feels mid-transition, right?
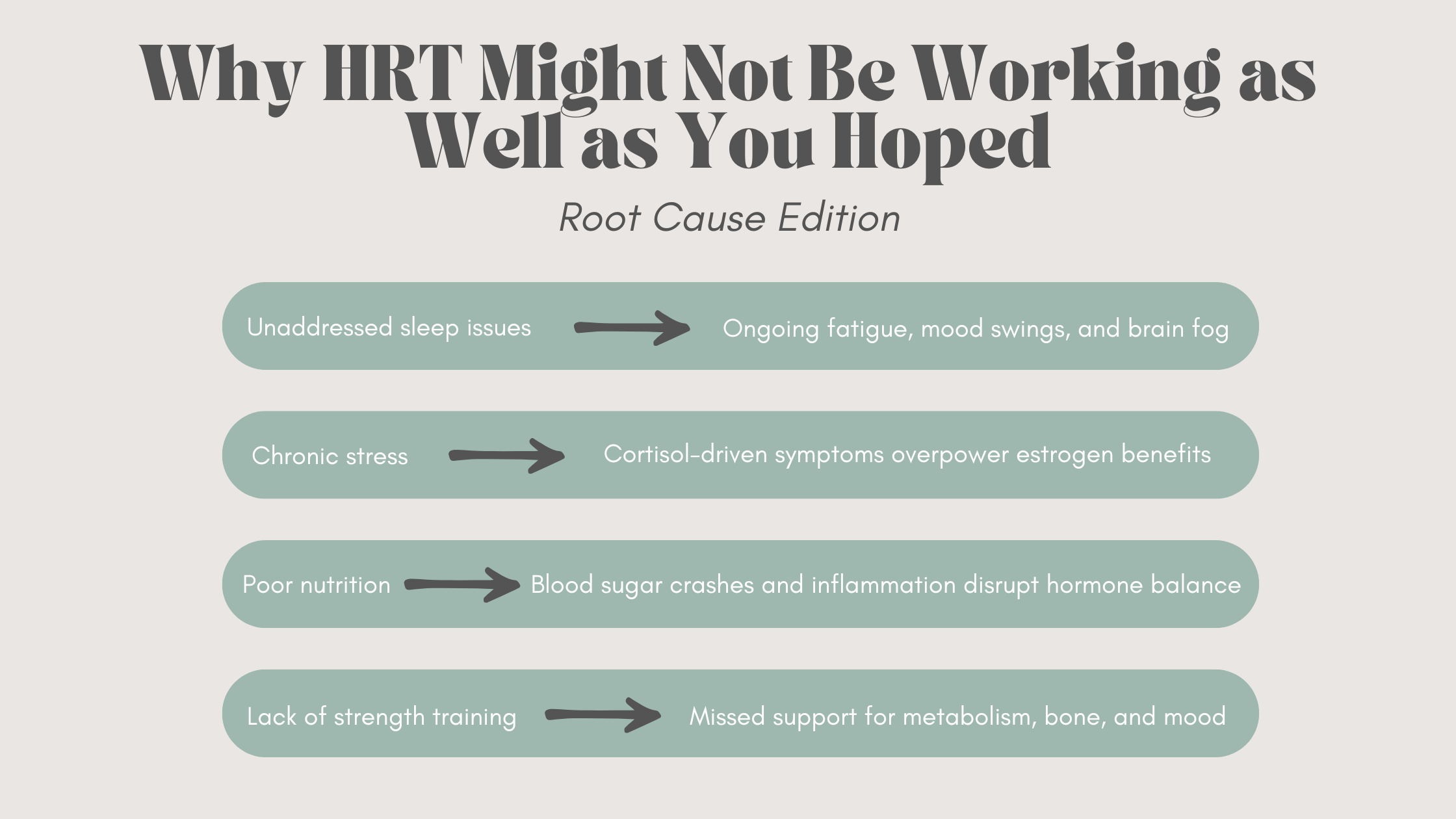
We talk about HRT like it’s the magic fix. And for some, it can feel like that. But menopause is not a single-issue condition.
It’s a whole-body, whole-life transition that affects everything from your bones and brain to your cardiovascular health, metabolism, and sleep.
Hormones can be the bridge—but the real work of long-term vitality lives in the foundations we build.
You Started Hormones. Now What?
This is one of the most common questions I get in practice:
“Okay, I’ve started HRT… what else should I be doing?”
And my answer is: plenty. Because while hormone therapy may relieve the symptoms, it doesn’t replace the habits that build resilience.
For example:
HRT helps you sleep → Now you have the energy to strength train for bone density
Hot flashes settle down → You finally have the capacity to dial in nutrition or start a walking routine
Mood stabilizes → You can return to the practices that regulate stress: mindfulness, boundaries, joy
Hormones make the lifestyle work more accessible, but they’re not the lifestyle.
Menopause Care Is More Than Symptom ManagementThat’s why I was so encouraged by the conversations happening at CMS this year.
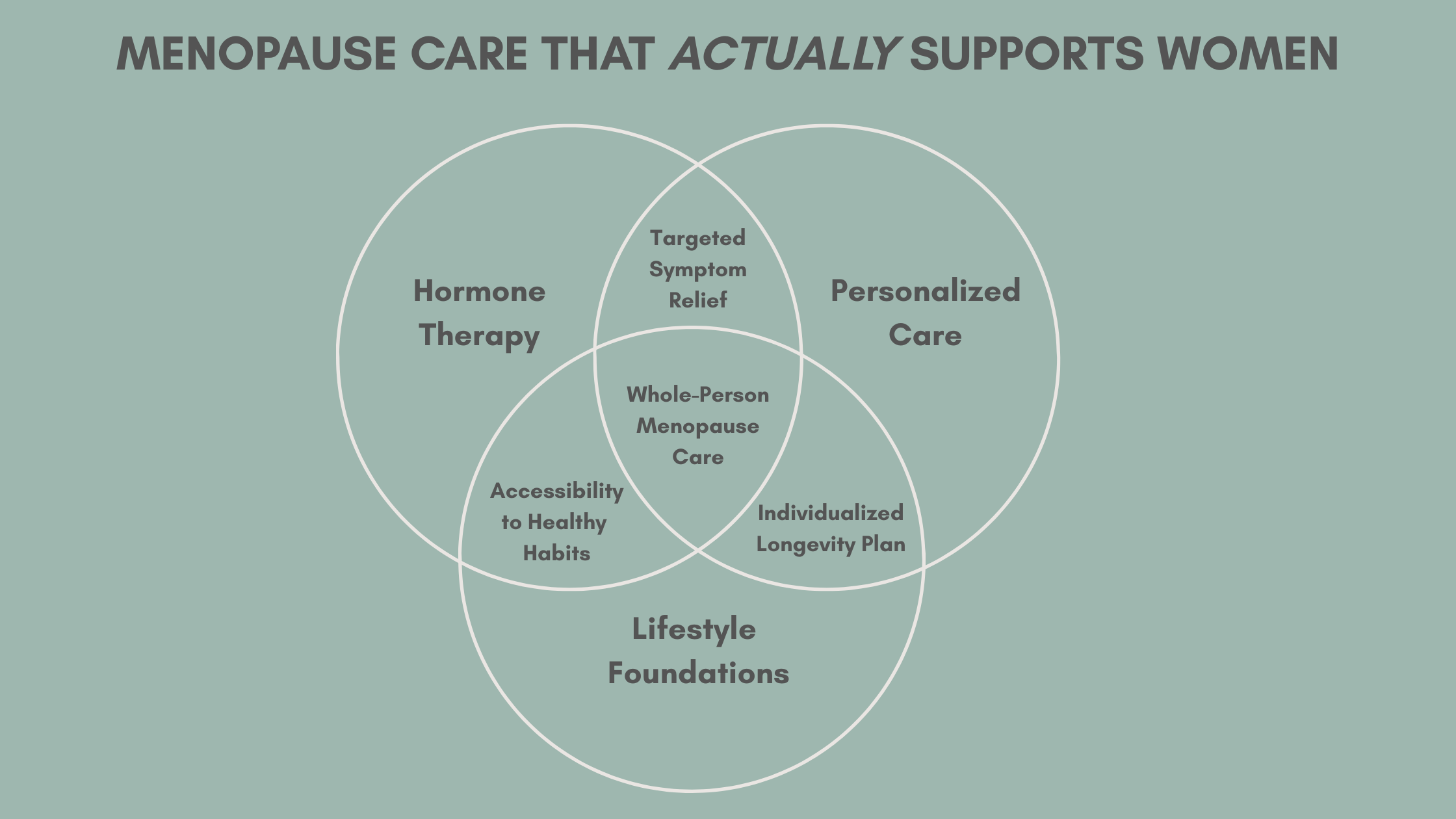
Let’s reframe what real menopause care looks like.
We don’t just chase symptoms.
We support the systems that create long-term health.
That means working on:
🛌 Sleep
Poor sleep worsens everything: mood, metabolism, memory, vasomotor symptoms.
Even without night sweats, many women struggle to stay asleep or wake up unrefreshed.
Sleep is predictive of long-term outcomes like cardiovascular disease and dementia.
We use strategies like CBTi, sleep hygiene, supplementation, and nervous system support to help restore restful sleep.
🧠 Stress Resilience
Chronic stress spikes cortisol, worsens hot flashes, increases belly fat, and hijacks your nervous system.
We support you with tools like breathwork, nervous system regulation, boundaries, and therapy—not just bubble baths.
🍽 Nutrition
This stage of life is a pivot point for blood sugar, cholesterol, and weight shifts.
We focus on:
Protein intake (especially for muscle and bone health)
Anti-inflammatory, whole-foods-based eating
Supporting healthy blood sugar and cholesterol
Calcium and vitamin D for bone health
🏋 Movement
If you’re not strength training in midlife, we need to talk.
Muscle is your hormone-supporting, blood-sugar-stabilizing, mood-lifting bestie.
Your exercise plan should include:
Resistance training 2–3x per week (bone + muscle)
Cardiovascular work (heart + brain health)
Mobility and flexibility (prevent injury and maintain independence)
🦴 Bone Health
Postmenopausal bone loss is real—and sneaky.
We build a prevention plan that includes screening, targeted nutrients, movement, and where needed, medication or specialized therapies.
❤ Heart Health
Cardiovascular disease is the #1 cause of death for women.
Midlife is when risk factors like high blood pressure, insulin resistance, and cholesterol often sneak in.
Your menopause care should include monitoring and prevention, not just symptom relief.
🧠 Cognitive Health
Brain fog is real, but it’s not always permanent.
We support cognition through sleep, blood sugar stability, physical activity, mental stimulation, and stress management.
💬 Mental Health & Mood
Perimenopause is often a time of increased anxiety, irritability, and low mood.
We screen and support women with counseling, lifestyle interventions, and when needed, medication or supplements.
💛 Sexual Health
Genitourinary Syndrome of Menopause (GSM) is underdiagnosed and often untreated.
Women deserve options like vaginal estrogen, lubricants, pelvic floor therapy, and real conversations—not shame.
What If Hormones Aren’t for Me?
Every woman deserves a conversation about hormone therapy.
But not every woman needs it, and not everyone can take it.
Some women have higher risk factors (e.g., breast cancer, clotting disorders).
Others simply don’t want it—and that’s okay.
The gold standard of menopause care is individualized care.
Your choices, your goals, your risk profile. Not just a one-size-fits-all protocol.
There are many evidence-based, non-hormonal options that can help with symptoms while still supporting long-term health.
“HORMONES can help you feel better. But the habits you build are what help you stay well.”
Final Thoughts: Hormone Therapy Is Powerful. But It’s Not a Solo Act.
If HRT gives you your sleep, libido, or energy back—amazing.
But real care goes further.
It looks like:
Checking your blood pressure and ferritin, not just your FSH
Talking about your resistance training goals, not just your night sweats
Thinking ahead to your 60s and 70s, not just surviving your 40s
What helps at 48 might not be what you need at 58. And your care plan should evolve with you.
Hormones are a tool. A powerful one.
But they’re not the foundation. You are.
📍 Started HRT and wondering what comes next? Let’s build your full roadmap for hormone support, longevity, and feeling like you again. Book a consult today—virtual care available across British Columbia.